What Is a Systems Approach to Examining a Patient
- Research article
- Open Access
- Published:
A proposed systems arroyo to the evaluation of integrated palliative care
BMC Palliative Care book 9, Commodity number:viii (2010) Cite this article
Abstract
Background
There is increasing global involvement in regional palliative care networks (PCN) to integrate care, creating systems that are more cost-effective and responsive in multi-agency settings. Networks are particularly relevant where different professional skill sets are required to serve the wide spectrum of stop-of-life needs. We advise a comprehensive framework for evaluating PCNs, focusing on the nature and extent of inter-professional collaboration, community readiness, and customer-centred care.
Methods
In the absence of an overarching structure for examining PCNs, a framework was developed based on previous models of health organisation evaluation, explicit theory, and the research literature relevant to PCN functioning. This research evidence was used to substantiate the option of model factors.
Results
The proposed framework takes a systems approach with organisation structure, procedure of care, and patient outcomes levels of consideration. Each gene represented makes an independent contribution to the description and assessment of the network.
Conclusions
Realizing palliative patients' needs for complex packages of treatment and social support, in a seamless, price-effective manner, are major drivers of the impetus for network-integrated intendance. The framework proposed is a starting time pace to guide evaluation to inform the evolution of appropriate strategies to further promote collaboration inside the PCN and, ultimately, optimal palliative care that meets patients' needs and expectations.
Background
Palliative intendance, back up to help those at end-of-life spend their remaining time in comfort and dignity, has evolved over time with improve agreement of the complex needs of those living with advanced illness and with growing acknowledgement of the importance of this health issue [i, 2]. Palliative care services tin exist provided in the habitation, hospitals, long-term intendance facilities, and hospices; ideally, within the context of ongoing assessment and management of the multiple physical, psychosocial, and spiritual facets of demand [3]. While non all dying people require or desire the aforementioned types of professional person palliative care services [four, 5], requests for interventions to alleviate both symptom distress and family caregiver burden are common in the last year of life [6, seven].
Providing the necessary complement of professional services to palliative intendance patients and their families in the community is a challenge in the current health care surroundings. The crumbling population and the changing epidemiology of serious chronic disease, coupled with the mounting costs of institutionalization [8] are straining wellness care systems [9, ten]. Community-based health services, such equally those for palliative intendance in the home, are frequently highly fragmented due to a combination of diverse professional groups, organizations, and approaches to intendance [11, 12]. A considerable torso of prove shows the prevalent under-identification of those in the palliative stage of disease who have significant distress (including pain and psychosocial conditions). It has been estimated that 60 to 80% of this population remains untreated for these concerns [6, thirteen].
Realizing dying peoples' needs for complex regimens of treatment and social support in a seamless, fiscally responsible way, and the difficulty of organizing these services in the community are major drivers of the impetus for multi-level strategies to amend coordinate palliative care. This has fuelled global involvement in integrated service delivery, involving the implementation of collaborative, responsive, toll-effective systems of care at the local level [14–16]. In many counties such as Canada, Netherlands, Australia, and the UK, these integrated systems of intendance have been mandated by formal policy initiatives in the class of regional palliative intendance networks [five, 14, 15, 17].
According to administrative sources on integrated commitment systems of intendance, namely Provan [12] and Shortell [18], these systems are divers by networks of health care organizations and professionals who work together to coordinate services to meet their patients' needs. Conceptually, these networks are a mode of linking fragmented services by increasing inter-organization interactions and ultimately maximizing system efficiency and seamlessness of patient transition [19, 11]. The integration of activities betwixt network agencies can include shared staff, joint policy development, articulation grooming programs or workshops, and shared information.
Relative to palliative care, service networks oftentimes germinate from informal arrangements between health intendance providers dedicated to serving the cease-of-life needs of those living in their communities. For the purposes of this paper, we define a formalized network equally a more evolved, organized system of intendance, as should be evident in the advent of government mandated structuring. At a minimum, this would correspond a membership-based group with multi-disciplinary representation from a variety of care settings. This network would exist overseen by an executive board or steering committee, enacted to provide leadership and direction in the local provision of palliative care services. Optimally, these palliative intendance systems include members with conclusion making and resource allocating authority, and representation from the community, academia, and healthcare institutions, operating with policies and data systems that are shared among providers within the network.
Although community-based network and collaborative palliative care squad objectives accept been delineated in the literature, there remains little explicit direction on how to operationalize these goals or how such initiatives should be evaluated [6, 20, 21]. Formalized health care networks, even with key structures such as resources and policy in identify, sometimes neglect to attain the goal of integration and ultimately, improvements in patient care. This is largely due to system barriers and poor interdependent functioning amid members, left unexamined [22, 23]. Superficial evaluations that rely on anecdotal or service apply information may be adequate for informing network development in the early on formative stages. However, once these networks go more than formalized with top-down involvement, this growing complexity necessitates a more comprehensive evaluative approach to competently identify system gaps.
With the increasing prominence of integrated service models in palliative intendance, and the precarious nature of these arrangements, at that place is a need for a comprehensive conceptual framework to better empathise the structure, procedure, and outcome functioning of these systems of care. While models of community illness management, such as Wagner'south Chronic Care Model [24] take been proposed, these are offered more broadly equally compendiums of principle components of a system of service, rather than as an evaluation framework. Furthermore, many of these disease care models have cocky-management and health orientations, non suited to a palliative intendance awarding. In the absence of an appropriate model to guide inquiry, the purpose of this paper is to offer, as a starting indicate, a multi-level evaluative framework for examining palliative care networks (PCNs) using a systems approach.
This newspaper begins with a presentation of our proposed framework and a general outline of the framework development procedure. This is followed by an introduction to the three-tier systems arroyo taken in this framework and an overview of the principal theoretical constructs included. Finally, the individual factors in the framework are described within each system level considered.
Framework Development
A conceptual framework explains the main things to be studied - the key factors, constructs, or variables - and the presumed relationships among them [25]. The framework we propose for examining palliative care system network functioning is presented in Figure 1. This framework focuses on describing the nature and extent of inter-professional collaboration, which is the central constituent of PCNs, but besides takes into account features of the prevailing health care surround. This framework is based on existing models and principles of health system evaluation, explicit theory, consideration of the empirical literature on determinants and indicators of inter-professional collaboration, and previous evaluations of palliative care systems. Constructs related to network success and sustainability, such as community readiness and client-centred care, take as well been integrated into the proposed framework.
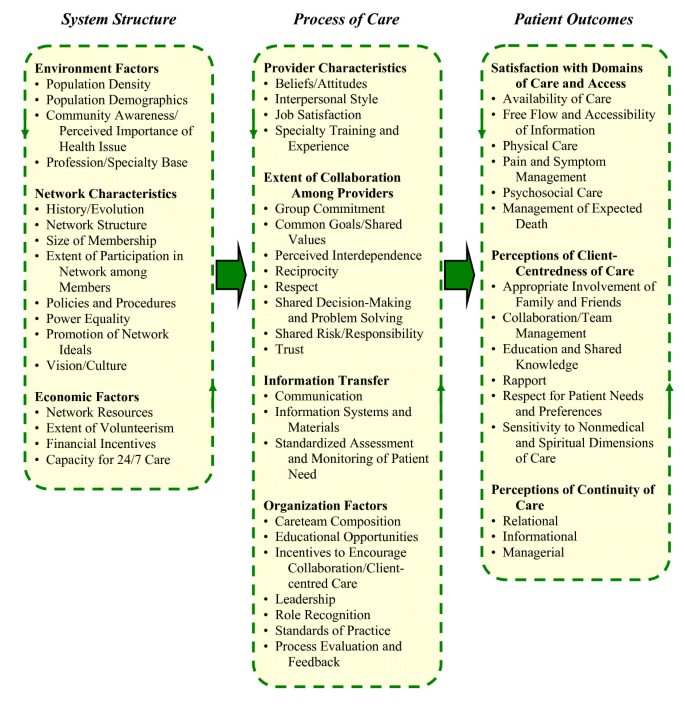
Conceptual framework for the evaluation of integrated palliative care networks.
This framework represents an affiliation of empirically-supported criteria, with each element making an contained contribution to the description and assessment of the network. Examining each element in the framework is of diagnostic value in that it tin can specifically direct where intervention is required to improve the overall system. Cardinal features of health arrangement evaluation reflected in the conceptual framework include the employ of theory-driven variables and a multi-tiered, systems approach. A theory-driven approach was employed to select potential predictor variables that were associated with the constructs of involvement because atheoretical studies are prone to excluding potentially important factors [25, 26]. In addition, the use of a theoretical framework to bulldoze the inquiry plan provides for a more systematic, valid, and empirically-sound method of study design, instrument evolution or option, and analysis.
A Systems Approach
The proposed framework is divided into System Structure, Processes of Intendance, and Patient Effect (SPO) levels of consideration originally represented in Donabedian'south S-P-O model [27]. This systems arroyo is frequently cited as a requirement of research on healthcare quality [28, 29], and is specially relevant to the exam of community partnerships [xxx]. In a health intendance context, 'Construction' is the availability of material and human resources, as well every bit, organizational characteristics and the physical, social, and economic environment nowadays. 'Process' refers to activities and transactions that constitute wellness care, usually carried out by professional personnel (but as well past non-professionals). Finally, 'Outcome' is the change in individuals attributable to the intendance they receive. These iii tiers are inextricably linked in that system structure contributes to processes, which in plow influence patient outcomes.
Evaluative research in palliative care provision typically focuses on either patient outcomes or provider perceptions of the process. To understand the underlying mechanisms to PCN functioning and in gild to be able to brand informed recommendations, requires a systems arroyo where the antecedents to processes and, in turn, patient outcomes are delineated. While the procedure level attributes may all-time capture network operations, construction features likewise need to be considered to understand the environmental characteristics that serve to enable or impede PCN processes.
Framework Basis
The full general influence of physical, social, and economic features of the wellness care delivery organization on patient outcomes has been described in Aday'southward [31] wellness system evaluation framework and Tarlov and colleagues [32] structural characteristics of care. These generic models delineating factors underlying the 3 tiers of healthcare (i.e., structure, processes, and outcomes) class the basis of our conceptual framework. To orientate this framework in terms of palliative care, this outline was supplemented by the inclusion of organization features from the Ferris and colleagues' [33] Square of Intendance and Organisation model of quality palliative care provision. Adult through a consensus-building procedure across Canada, this model too takes a S-P-O approach, specifying attributes that should fall under each intendance level, from Resources and Functions (i.e., structure), to Procedure, to Common Patient Problems (i.eastward., outcomes) within the palliative intendance organization. Upon this palliative intendance organization base architecture, the principal constructs of relevance to network functioning are overlaid to create the proposed evaluative conceptual framework. These constructs are: member collaboration, community readiness, and client-centred intendance.
Principal Constructs in Framework
In that location are iii central constructs interwoven throughout the framework that are integral to PCN functioning, namely collaborative care, community readiness, and client-centred care. Each of these constructs is described in particular below.
Collaborative Care
Inter-professional collaboration where physicians and other health care providers piece of work in partnership to deliver comprehensive and profession appropriate care has gained the attending of policy makers nationally and internationally and has get a priority in near health intendance reforms [21, 34–38]. The desired immediate issue of PCN formation is the growth of inter-professional provider collaboration [14]. There can be no integration of health care without collaboration; accordingly, consideration of the features of this construct need to be at the core of an examination of these organized networks.
The advantages of a collaborative approach utilise extensively to palliative care, where different professional skill sets are required to serve a wide spectrum of patients' needs [11, 39]. Meta-analyses have confirmed the benefits of collaborative care, with palliative patients and their families reporting greater satisfaction with wellness services and better pain and symptom management, as well equally improvement in the timeliness of services through expedition of the referral process [2, twoscore–42]. Cost reduction has as well been cited equally an result of collaboration by reducing the corporeality of time patients spend in acute infirmary settings.
Some ambiguity exists in the literature surrounding the term inter-professional person wellness intendance [21, 43]. The prefix 'inter' refers to a partnership where members from dissimilar professions piece of work collaboratively towards a mutual purpose. These partners come together to share ideas, skills, and knowledge to structure a collective action towards the patient'due south care needs [21, 44]. In a multi-disciplinary squad, the professional identity and ranking of individual team members usually supersedes squad affiliation, whereas in the inter-disciplinary (i.e., inter-professional) team the identity of the squad is principal.
Rather than a traditional hierarchy where a medico directs care, in a collaborative approach unlike team members may assume leadership depending on the patient's needs [half-dozen]. Physicians, nurses, and other health intendance providers have complementary clinical and therapeutic skills, and different perspectives on problems the palliative patient might run into. With these combined competencies, the inter-professional person squad is more responsive to the configuration of intendance delivery required, reducing the complication of accessing health and social care for patients in demand [3]. Synergy is oftentimes a defining feature of high functioning collaborative teams, with favourable outcomes possible from collective competences being greater that the sum of the team parts [45, 46].
A theoretical model of collaboration should showroom an understanding of the many elements of the construct and the components influencing the process, at multiple structural levels. Although the health care literature is replete with theoretical frameworks of collaboration, with 29 different models solitary reported in a 1995 review [47], no single model lends itself to a comprehensive, practical application and none were designed specifically for palliative care. The majority of published piece of work on the inter-professional collaboration construct relies on conceptual approaches rather than on empirical information [half-dozen, 48]. This litany of untested frameworks cloud perceptions of exactly which interventions improve collaboration between health intendance professionals, the influence of determinants on collaboration, and central factors to sustainability [20, 49, 50]. Identification of the key components of collaboration requires comparison and contrast of the systematic review literature examining this construct, bachelor largely from primary care and chronic care contexts.
Community Readiness
The Customs Readiness Model is a theory-based approach to ascertaining the favourability of the social and political climate in a given setting to program implementation [51]. This model has been used in international contexts, often to betoken community receptivity to prevention or substance apply initiatives [52]. However, community readiness can also be accordingly practical to the planning of community-based health interventions, to predict program sustainability and every bit a tool for program evaluation.
This model is related to the more ordinarily cited organizational readiness concept [53, 54], however, community readiness goes beyond the telescopic of a single institution in considering multiple organizations, determination makers, and consumers. The style in which health issues are divers and dealt with is often intertwined with customs and cultural norms [51]. Attempting to alter established conventions of health care exercise and construction can present a formidable barrier, only equally the inertia of traditional care provider roles tin impede efforts to increase system integration [55]. In considering community readiness for PCN initiatives, it is important to establish if adequate chapters and support in the general community and between providers and their organizations exists for promoting the network's ideals. Organization organisation, provider educational activity, and policy must all be appropriately aligned to maintain a supportive environment for wellness professionals practicing inter-disciplinary care.
In many respects, process level factors which imply the state of readiness and shared resolve towards collective action, such as the commitment, attitudes, and goals of both providers and their leaders towards PCN objectives, transcend into the other two primary constructs in the framework: collaborative care and client-centred intendance. Assessing elements of customs readiness, both in system structure and intendance processes, are an important tenet of predicting the viability of a community palliative intendance initiative [56]. If a low phase of readiness is indicated, changes proposed by this plan are likely to see resistance, illuminating the need to first attend to whatsoever model elements identified as underdeveloped.
Client-centred Intendance
Client-centred care refers to the provision of care that is respectful of and responsive to private patient values, needs, and preferences [57]. This includes viewing patients holistically and allowing their unique perspectives to guide care decisions, enabling them to human action as a central resources in their own wellness [58]. Even though the care provider may exist the expert clinically, to deliver intendance that is client-centred requires edifice a human relationship with the patient that facilitates the self-identification of personal goals, to ensure the giving of information and directly intendance that is appropriate, timely, and pertinent to the client'south wishes [59].
Client-centred care has become a central principle of nursing practice in most developed countries and has too been adopted by other health professions [59–62]. This arroyo has been found to positively bear upon the satisfaction of both the patient and the provider in chief health intendance [63]. Likewise, care that is patient focused is vital to the success of patient education and support strategies intended to encourage successful emotional and practical adaptation to advanced chronic illness [58]. Client-centred care has definite applicability to palliative intendance in the community where support is provided based on the unique circumstances of patients to all-time sustain their quality of life.
Conceptual Framework Domains
The components of the framework as presented in Figure 1 are described in the sections that follow. Rationale and empirical back up are given for the inclusion of each framework element. This clarification is organized past arrangement level (South-P-O), with explanation provided for each domain (and sub-domain) within each level.
Organization Structure Domains
Environment Factors
Environment factors are the characteristics of the geographic area or region in which the network system of interest is located. These factors include population demographics such as historic period distribution, income levels, indigenous composition, and cancer mortality rates for the area (meet Figure 1). Population density in terms of urban and rural distribution can also have implications for service delivery [56]. Creating a profile of the system environs provides context for comparing to other networks, too as enabling generalizability of the results to other similar environments.
The capacity for change within the environment largely rests upon the readiness of those living in the planning region'south customs, including policy makers and consumers. The level of community awareness of both the health care issue, e.g., palliative care needs, and the efforts being made to address this problem, as well as the attitude in the community towards the upshot, are main considerations in predicting the success of directed programs [56]. A lack of support in the population for a new initiative can undermine the confidence of providers involved in implementation. A network structure introduced despite community indifference or reservation, which tin can include opposition by influential organizations, is likely to fail [46, 64]. Another prerequisite for a successful PCN is the presence of an adequate puddle of nurses, physicians, and allied wellness care workers with some specialization in palliative intendance.
Network Characteristics
Characteristics of the PCN itself likewise provide context and betoken organisation level barriers and facilitators to the achievement of the network's goals and, effectively, optimal outcomes for palliative intendance patients. Factors to be considered are the PCN'southward history, development, structure, formal/informal policies and procedures, and vision/civilisation and whether these aspects promote connected growth of the network and a collaborative environment [33, 43, 45, 48, 53, 56, 65]. The number of health care providers, administrators, and other relevant disciplines in the region holding membership in the PCN (size of membership), the extent of participation of these members in network functions, and the promotion of network ideals internally and throughout the community, all speak to the influence, stability, and perceived value of the PCN. Cooperation between the relevant organizations in the system and their positive regard for the PCN ratifies the delivery of these organizations' employees at a process level. Organizations that take traditionally had substantial command over healthcare resources and service planning may exist unwilling to relinquish this ability to have co-dependence, limiting network cohesion [xiv].
Policies and procedures demand to reflect clearly delineated obtainable objectives and goals [53, 65]. These utilize to network development, just likewise instilling essential features of holistic palliative intendance. Specifically, this includes policies for consistently offering patient-focused care, home death as a viable pick, and expected death planning [66]. A final structural quality is the caste of power equality among network members. As previously mentioned, the authority given to each particular professional person discipline inside the network needs to be equitable to encourage member contribution and support collaborative patient care [48].
Economic Factors
Sufficient resource and infrastructure are required to make whatsoever health program sustainable and adaptive [43, 53, 56, 67]. These avails include greenbacks, financial investments, skilled professionals, equipment, office space, and technology [33]. The availability of designated facility-based programs, namely hospice spaces and palliative intendance unit of measurement beds in 3rd centres, is vital to meeting higher levels of need and providing respite for family caregivers. Liabilities that the PCN carries, such equally loans or insurance payments, as well need to be considered. The extent of volunteerism contributing to either care provider or authoritative functions further increases the PCN'southward majuscule. Financial incentives are the provision of resources tied to the uptake of a specified approach and/or the meeting of ready requirements. Incentives aligned with network development provide motivation and legitimacy to this endeavour and therefore need to exist noted.
An essential component to palliative intendance access not found within the constructs considered, that has emerged from review of multiple models of palliative care provision reported in national research documents [68], and as a constituent of integrated care [69], is the system's chapters to offer care 24 hours per solar day, vii days per week (24/7 care) in each of the relevant professional disciplines. The availability of around-the-clock care is essential to adequately accost customs palliative care problems such as caregiver fatigue and end-of-life pain and symptom management [66]. Without the availability of 24/vii professional intendance, crises may ascend which consequence in patient transfer from domicile to emergency/acute care facilities.
Process of Care Domains
Provider Characteristics
Although inter-professional collaboration and other contributing factors to quality palliative care may be encouraged under the auspices of network structures, these orientations are largely voluntary by nature. Uptake is influenced by the personal characteristics of service providers and administrators in the group [21]. Many of the elements of this domain are contained in Tarlov and colleagues [31] systems of health intendance model (see Figure i for framework). Provider characteristics and other process level factors also speak to readiness among the "customs" of network members for integrated palliative care [56].
Beliefs and attitudes of PCN participants are ideally congruent with those of collaborative client-centred practice in members viewing this endeavour every bit worthwhile and being motivated towards this end [21, 53, 65, 67, seventy, 71]. Interpersonal style refers to professionalism amongst network members, which ultimately determines the caste to which professionals are able to work together [21, 45, 65, 72, 73]. Pertinent interpersonal factors include collegiality, the power to clear beliefs and communicate effectively, personal maturity, self-reflection, assertiveness in presenting one's own professions' perspectives with confidence, and willingness to cooperate rather than compete. Job satisfaction, bolstered by a favourable piece of work surroundings, is a stiff predictor of provider commitment to their function [45, 48, 70, 71]. Another fundamental characteristic is specialty preparation, representing the professional education and skills of members. The amount of time spent as a palliative care provider and as a network participant are likewise important considerations [21, 45].
Extent of Collaboration among Providers
Prior examination of inter-professional teams have shown that collaboration is a complex and dynamic process [21]. While there is a lack of a single definitive model of palliative care inter-professional collaboration to guide a comprehensive evaluation [74], there is some understanding in recent systematic reviews about the key factors inside this construct that influence and/or betoken the state of collaborative practice [21, 43, 45, 48, 65, 67, 70, 72, 75].
Procedure level factors consistently mentioned in the literature equally suggesting the extent of collaboration among providers, are group commitment, common goals/shared values, perceived interdependence, reciprocity, respect, shared controlling and trouble solving, shared risk/responsibility, and trust. These qualities are also consistent with the prerequisites for supporting client-centred intendance processes. In fact, some studies interrelate this latter construct with that of collaborative care, such that collaboration leads to desirable client-centred intendance outcomes [45, 73].
Overall group delivery to collaboration and to quality intendance more than broadly is one of the most important contributing factors to team functioning and network stability [21, 45, 48, 56, 70, 71, 75]. The common goals and shared values sub-domain necessitates members establishing a common language, similar realities and norms, and clear objectives, also as a team task orientation. The latter implies a commonage commitment to excellence in task performance in collaborative customer-centred care with minimal conflict [21, 45, 47, 65, 67, 71, 72, 75].
Perceived interdependence is apparent in team orientation and working relationships among community providers [45, 47, 56, 65, 71, 72, 75]. Having an interdisciplinary team base of operations where team members can work in shut physical proximity to ane another contributes to interdependence potential. Reciprocity refers to the perceived benefits of network interest for each member weighed against the negative consequences and that in that location are noticeable returns with increasing collaborative efforts [72, 76]. Mutual respect implies an appreciation for dissimilar professional perspectives and that the contributions of each are valued [21, 45, 47, 48, 65, 72, 75, 77]. Shared decision-making and problem solving is evidenced in solutions derived through an integration of the expertise of each professional [45, 47, 71, 72]. Furthermore, decisions should be based on general consensus, so that all disciplines feel empowered.
Shared risk and responsibility pertains to the accountably for joint initiatives being fairly distributed, with members sharing in the liability for innovations involving risk [21, 45, 47, 65, 70, 72, 77]. Finally, a high level of common trust within the PCN is quintessential to members working effectively together [21, 45, 47, 48, 65, 70, 72, 75, 77]. This element infers confidence in others and trusting 1's own abilities.
Information Transfer
Communication pervades all aspects of provider collaboration and patient-centered interactions. Activities that stimulate advice between professionals such as regular formal and informal interdisciplinary forums are crucial to collaboration between individuals and between their organizations, which in turn enhances the quality of palliative care [xiv]. The sharing of information that is relevant, accurate, transparent, curtailed, and timely is an essential element for reaching a common understanding across professional boundaries and for effective negotiations within the network [21, 45, 47, 48, 65, 71–73, 75, 77]. The ability and willingness of providers to engage clients in a dialogue unique to their needs and care options captures patient-centred communication from a procedure level.
Information systems and materials are mechanisms to facilitate the exchange of data. Systems include technologies such every bit pagers, smartphones, electronic health records systems, and multidisciplinary case videoconferencing [43, 45, 77]. Materials refer to written and visual aids to assist learning, decision making, and uptake of guidelines, network values, and activities. Standardized tools for documenting and transferring information such every bit an in-home patient chart, besides foster effective communication.
Related to informational mechanisms are those for standardized cess and monitoring of patient demand. These mechanisms refer to useful clinical tools and assessment instruments and the adoption of these into broader organized approaches within the PCN. Such practices are essential in ensuring that palliative care needs in the community are uniformly identified and that bachelor resources are accessed efficiently [33, 68, 78].
Organization Factors
Organizational factors identified as process determinants of collaborative client-centered care are care squad limerick, educational opportunities, incentives to encourage collaboration/client-centred care, leadership, role recognition, standards of practise, and process evaluation and feedback. Care team composition refers to the appropriateness of skill mix present in the PCN and having the right people involved both in terms of the expertise they bring to the group but also the influence they accept in the community [21, 56, 65, 71, 75]. Educational opportunities consist of training and workshops, the provision of technical help, and venues providing professionals the opportunity to learn from one some other [21, 71, 45, 48, 79]. Incentives to encourage collaborative client-centred care and quality care in general include recognition for innovation and excellence, squad building exercises, and fourth dimension protected for network specific responsibilities. The formalization of these inducements confirms the commitment of executive members to network evolution [21, 71, 75]. Research indicates that incentives to encourage collaborative practice are more than effective when administered to the squad equally a whole rather than separately to individuals within the team [71].
Leadership is frequently cited as the single most important cistron contributing to collaborative customer-centered intendance. Leaders need to inspire and oversee the other positive process constituents of network functioning and aid resolve conflicts that arise [21, 46, 48, 65, 71, 75, 76, 79]. Weakness in this role can erode PCN cohesion. Role recognition speaks to function clarity in that the contribution of each member is understood, besides equally their roles being valued [21, 45, 48, 65, 67, 71]. Standards of practice are benchmarks by which team members can compare electric current and target values for indices of inter-professional working, client-centred intendance or other functioning qualities [21, 45, 48, 80]. Finally, process evaluation and feedback has also been indicated as an essential factor to sustaining network relationships [21, seventy, 75, 79, 80]. Quality management systems for ongoing evaluation and modification of operation through the review of network activities, functions, and outputs are disquisitional for improving efficiency and enhancing the patient experience.
Patient Upshot Domains
Satisfaction with Domains of Intendance and Access
The consideration of patient outcomes in the proposed framework does not delve into case complexity, such every bit functional dependence, which can vary greatly independently of intervention [81]. Rather, this level focuses on the reaction of the palliative intendance organization to needs from patients' points of view. The impact of inter-professional collaboration would be assessed by patients' perceived quality of care and satisfaction with the care they received. A cluster assay of aspects of palliative intendance satisfaction in the literature resulted in four dominant sub-domains emerging: availability of care, information giving, concrete intendance (including pain and symptom management), and psychosocial intendance [82]. These factors, along with management of expected decease, have been identified every bit the core elements in describing palliative care processes from the intendance recipient's perspective [21, 33, 42, 70] (meet Figure 1).
Availability of care simply denotes the perception that services were accessible to those who needed them, when they needed them. The free flow and accessibility of information to the patient has too been identified as a central feature of client-centered care [79]. Physical care involves medical and practical aspects of intendance, but also pain and symptom direction which in this framework has been designated as a separate sub-domain given its importance in palliative care [33]. Psychosocial care involves coming together the emotional, psychological, and existential needs of palliative care patients and their families, in helping to alleviate grief, fear, and other psychological and social problems. Finally, management of expected expiry refers to the initiative that providers take to assistance family caregivers so that life closure preparations, death pronouncement, certification, and other necessary arrangements occur with lilliputian difficulty upon the passing of the palliative private [33].
Perceptions of Client-Centredness of Intendance
A systematic review by Shaller [79] of ix frameworks for defining client-centered care resulted in the identification of the post-obit core elements of this construct: appropriate involvement of family and friends in decision making and information giving; the sense of inter-provider collaboration and squad management; education and shared noesis in terms of timely and consummate information on patient prognosis, progress, and disease process;respect for patient needs and preferences in intendance; and sensitivity to nonmedical and spiritual dimensions of care. The end-of-life patient and his/her family perceiving the presence of these factors in interactions with health intendance providers would imply that intendance is client centered. Furthermore, this would be particularly axiomatic in patients feeling that care professionals had attempted to build a rapport with them, which in turn fostered qualities of interdependence, including trust [58, 83].
Perceptions of Continuity of Care
An overview by Haggerty, Reid, and McKendry [84] identified the following three types of continuity of care: relational continuity (patient seeing usual practitioner); advisory continuity (advice and cognition where patient information flows easily between involved intendance providers); and management continuity (coordination of care so that transition between intendance providers is clear and seamless for the patient). Each of these facets of continuity is another positive event facilitated by collaborative relationships between providers, the end event of which should be credible to patients and their family caregivers [43, 45, 70]. Accordingly, continuity of care is a miracle best measured from the perspective of the patient. Patients' perceiving that efforts had been fabricated past providers to make the care process flow smoothly (management continuity) is as well an aspect of intendance that is client-centred [85].
Discussion
Evaluation and feedback plays a key office in developing organized systems of intendance [thirty, 75, 80]. Evaluation tin make up one's mind the extent to which program objectives are met, inform policy and planning decisions, and increment community awareness and support for an initiative. Although critical, evaluation can be costly in terms of staff time and funding, and therefore is often deferred in favour of using these resources for providing care [xxx]. This may explicate why the literature is lacking in intendance delivery research in palliative care [86]. With growing involvement in amend integrated services for those at end-of-life, there is a global demand for whole arrangement research in palliative care that captures the complexity of these initiatives. However, no evaluative framework exists for explicitly examining a network organized organization of care in this context.
In this manuscript nosotros have proposed an overarching construction for examining palliative care networks (PCNs) that can be applied to a system evaluation. Findings emerging from such an exercise would be of utilise to planners, administrators, and advocates of integrated palliative care systems, for the purposes previously mentioned. This paper represents an important initial effort to outline a conceptual map of the organisation structure, process of care, and patient upshot (S-P-O) domains for organizing systems of care for those in the palliative phase of life who are residing in the community. Research evidence was used to substantiate the pick of model factors. Our focus has been on inter-professional collaborative palliative practise, client-centred intendance, and community readiness constructs; taking into business relationship contextual factors to capture the unique features of the system environs. Many of the elements derived from these constructs overlap, indicating their interdependence.
This model does not incorporate specific palliative care practices, as accept been proposed by intervention guidelines such as the Liverpool Care Pathway [87]. Nor have we considered private patient and family characteristics, which often play a decisive role in patient and caregiver outcomes [88], but yet likely reverberate intrinsic attributes and dispositions that are less modifiable through formal support interventions [89]. Instead our framework is built effectually features of importance to PCN functioning, with provider and patient contexts. Many of the factors contained herein could as well exist suitably applied to the test of integrated community systems for the management of other diseases.
In terms of application, the proposed framework assumes the employment of a mixed-methods research programme. This implies using multiple sources of data to consider the different perspectives and Southward-P-O levels inside the PCN organization. Mixed-method enquiry is usually advocated to provide for a broader range of questions, leading to a more consummate understanding of the phenomena of study - in line with a systems approach [xc, 91]. Compared to single method studies, stronger evidence is possible through using mixed-methods in the convergence and corroboration of findings, with the results having greater generalizability. A instance study methodology is 1 type of mixed-methods blueprint that complements the proposed framework [92, 93].
At the structure level, information would be obtained from PCN administrators and document review (east.g., coming together minutes, presentations, etc.). Data drove at the process level would need to include members of the PCN providing care, these beingness specialist nurses, chief care and palliative intendance physicians, pharmacists, therapists, and social workers [6, 94–96]. As for patient outcomes, obtaining responses from palliative individuals can be challenging [81, 97, 98]. Equally such, it may be prudent to collect data from the primary family caregiver rather than the patient directly to gain insight into intendance outcomes in the community [99]. A cistron matrix based on the questionnaire items adult from the conceptual framework should be created to ensure consummate coverage of desired elements and to assist in analysis for mapping individual factors relative to one another. Visually depicting the data in an organized array is a useful step in progressing theme germination and in discerning relationships between the structure, provider, and patient levels of the system.
While comprehensiveness is a forcefulness of this proposed conceptual framework, it can too exist a limitation in the breadth being maybe as well extensive for the practical evaluative needs of a PCN. In translating the framework into an evaluation research plan, attempting to consider all the dimensions and numerous factors at once tin can make operationalization a challenge, especially if fourth dimension and resources are limited. Evaluators, especially health intendance providers taking on this office in addition to their clinical responsibilities, should avoid making data drove too burdensome [80]. Whether it is a quondam snapshot of the network or the implementation of an ongoing surveillance mechanism, it may be advisable to start small to avert the process condign unmanageable and subsequently beingness abandoned entirely. Depending on the objectives of the inquiry, the size of the program, and the resident experience nowadays, researchers may prioritize select elements to be included as sentry indicators, to focus measurement efforts.
I approach to a more than pragmatic examination is to limit the inquiry to issues at the patient level and then trace problems that sally back to the processes of care to isolate and nourish to contributing factors. Alternatively, a selection of factors at the process level could be assessed by using an existing validated tool that captures some of the domain(s) of interest. For instance, the full general country of inter-professional collaboration could be determined using an established instrument such as the Partnership Cocky-Cess Tool (PSAT) [46], which is regarded as one of the better instruments to measure out this construct [72] and includes a reporting module for interpreting and disseminating the results. Further testing of the proposed model may reveal a fix of cadre indicators in network functioning and outcomes that lend themselves to the creation of a condensed version of the model, for guiding a bones evaluation of a PCN.
A network approach to service provision does non necessarily assure the best care for patients, peculiarly if health intendance funding streams continue to exist competitive and encourage provider organizations to be territorial. A system driven past a single authority could potentially be more than efficient and produce better outcomes than a cooperative arrangement, by dissolving organizational boundaries. Still, given the diversity of providers and organizations providing care to end-of-life patients and their families in many communities and the variable needs of this patient population, attempting to integrate existing programs seems a more viable solution. The provision of palliative intendance that is client focused needs to exist the grounding objective in service integration to assistance refocus some of the territoriality that arises as individual organizations try to protect their own interests [14].
Conclusions
Information technology is important to retrieve that arrangement integration, still advantageous, takes a long time to attain [46, 100], requiring resources and the participation of the total range of palliative care providers, from hospitals to contained practitioners. The conceptual framework proposed contains a multiplicity of key factors to palliative care system functioning. This is a starting time step to guide evaluation to inform the development of appropriate strategies to further promote collaboration within the PCN and, ultimately, optimal palliative care that meets patients' needs and expectations.
References
-
Canadian Hospice Palliative Care Association: What is palliative intendance?. [http://world wide web.chpca.net/top_menu_items/faqs.html]
-
World Wellness System: Meliorate palliative care for older people. 2004, [http://www.euro.who.int/document/E82933.pdf]
-
Coyle N: Interdisciplinary collaboration in hospital palliative intendance: Chimera or goal?. Palliat Med. 1997, eleven (4): 265-266. 10.1177/026921639701100401.
-
Franks J, Salisbury C, Bosanquet N, Wilkinson EK, Lorentzon Thou, Kite S, Naysmith A, Higginson IJ: The level of demand for palliative care: A systematic review of the literature. Palliat Med. 2000, 14 (ii): 93-104. 10.1191/026921600669997774.
-
Palliative Care Australia: A Guide to Palliative Care Service Evolution: A Population Based Approach. 2005, Palliative Care Australia, Deakin
-
Abu-Saad HH: Evidence-based Palliative Care Across the Life Span. 2001, Oxford: Blackwell Science Ltd
-
Lim JW, Zebrack B: Caring for family members with chronic concrete disease: A disquisitional review of caregiver literature. Health Qual Life Outcomes. 2004, 2 (50): 1-9.
-
Korabek B, Slauenwhite C, Rosenau P, Ross L: Innovations in seniors' intendance: Habitation care/medico partnership. Canadian Journal of Nursing Leadership. 2004, 17 (three): 65-78.
-
Carstairs South: Still Not In that location. Quality End-of-Life Care: A Progress Study. 2005, Ottawa: Senate of Canada
-
U.S. Department of State, Department of Health and Human Services, National Institute on Aging, National Institutes of Health: Why Population Crumbling Matters: A Global Perspective. Washington DC. 2007
-
Lemieux-Charles L, Chambers LW, Brazil K, Cockerill R, Jaglal S, Le Clair JK: Dementia Care Networks' Written report. 2002, Ottawa: Canadian Wellness Services Research Foundation
-
Provan KG, Sebastian JG: Networks within networks: Service link overlap, organizational cliques, and client outcomes in community mental health. University of Direction Journal. 1998, 41 (4): 453-463. 10.2307/257084.
-
Reb AM: Palliative and end-of-life care: Policy analysis. Oncol Nurs Forum. 2003, 30 (1): 35-fifty. x.1188/03.ONF.35-50.
-
Nikbakht-Van de Sande CV, Rijt van der CC, Visser AP, 10 Voorde MA, Pruyn JF: Function of local networks in palliative care: A Dutch view. J Palliat Med. 2005, 8 (iv): 808-816. 10.1089/jpm.2005.8.808.
-
Travis S, Chase P: Supportive and palliative care networks: A new model for integrated care. Int J Palliat Nurs. 2001, 7 (10): 501-504.
-
Vanderbent S: Strategies for transition planning in Ontario's Local Health Integration Networks. Healthc Q. 2005, 8 (3): 78-81.
-
Dudgeon D, Vaitonis V, Seow H, King S, Angus H, Sawka C: Ontario, Canada: Using networks to integrate palliative intendance province-wide. J Pain Symptom Manage. 2007, 33 (5): 640-644. 10.1016/j.jpainsymman.2007.02.001.
-
Shortell SM, Gillies RR, Anderson DA, Mitchell JB, Morgan KL: Creating organized delivery systems: The barriers and facilitators. Hosp Health Serv Adm. 1993, 38 (iv): 447-466.
-
Brazil M, Bainbridge D, Sussman J, Whelan T, O'Brien M, Pyette N: Providing supportive intendance to cancer patients: A study on interagency collaboration. Int J Integr Care. 2008, 8: 1-9.
-
Corner J: The multidisciplinary team: Fact or fiction?. Eur J Palliat Care. 2003, 10 (2): 10-thirteen.
-
Oandasan I, Baker GR, Barker K, Bosco D, D'Amour L, Jones South, Kimpton Southward, Lemieux-Charles 50, Nasmith L, San Martin Rodriguez L, Tepper J, Way D: Teamwork in Healthcare: Promoting Effective Teamwork in Healthcare in Canada. 2006, Ottawa: Canadian Health Services Research Foundation
-
Farrell M, Schmitt M, Heinemann Grand: Informal roles and the states of interdisciplinary team evolution. J Interprof Care. 2001, 15 (30): 281-295.
-
Reed J, Cook G, Childs S, McCormack B: A literature review to explore integrated care for older people. Int J Integr Intendance. 2005, 5: ane-8.
-
Wagner EH, Austin BT, Davis C, Hindmarsh K, Schaefer J, Bonomi A: Improving chronic illness care: Translating testify into action. Health Aff. 2001, xx (6): 64-78. 10.1377/hlthaff.20.6.64.
-
Miles MB, Huberman AM: Qualitative Data Assay an Expanded Sourcebook. 1994, Thousand Oaks, CA: Sage Publications, 2
-
Brazil K, Ozer Due east, Cloutier M, Levine R, Stryer D: From theory to practice: Improving the impact of health services inquiry. BMC Health Serv Res. 2005, five (ane): 1-ten.1186/1472-6963-5-1.
-
Donabedian A: Evaluating the quality of medical intendance. Milbank Mem Fund Q. 1966, 44 (one): 166-203. 10.2307/3348969.
-
Burns LR: Medical organization structures that promote quality and efficiency: By research and future considerations. Qual Manag Wellness Care. 1995, three (4): 10-18.
-
Found of Medicine: Health Services Research. 1979, Washington DC: National Academy of Science
-
Butterfoss FD, Francisco VT: Evaluating community partnerships and coalitions with practitioners in mind. Health Promot Pract. 2004, five (2): 108-114. 10.1177/1524839903260844.
-
Aday LA: Institution of a conceptual base for health services research. J Wellness Serv Res Policy. 2001, half dozen (3): 183-185. ten.1258/1355819011927332.
-
Tarlov AR, Ware JE, Greenfield Due south, Nelson EC, Perrin East, Zubkoff Thou: The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989, 262 (vii): 925-930. 10.1001/jama.262.seven.925.
-
Ferris FD, Balfour HM, Bowen K, Farley J, Hardwick M, Lamontagne C, Lundy M, Syme A, West P: A Model to Guide Hospice Palliative Intendance: Based on National Principles and Norms of Practice. 2002, Ottawa: Canadian Hospice Palliative Care Association (CHPCA)
-
Commission on Medicare: Caring for Medicare: Sustaining a Quality System. 2001, The Commission on Medicare, Regina
-
MacLean MJ, Kelley ML: Palliative Intendance in Rural Canada. 2002, Regina: University of Regina
-
Nanchoff-Glatt One thousand: Collaborative health intendance: A personal perspective. 2003, [http://world wide web.cfpc.ca/English/cfpc/education/department%20of%20teachers/new%20teachers/Michele%20Nanchoff%20Glatt/default.asp?southward=1]
-
Senate of Canada: Quality Terminate-Of-Life Care: The Right of Every Canadian. Ottawa. 2000
-
Sicotte C, D'Amour D, Moreault M: Interdisciplinary collaboration within Quebec community wellness care centres. Soc Sci Med. 2002, 55 (6): 991-1003. 10.1016/S0277-9536(01)00232-5.
-
Leichsenring K: Developing integrated health and social care services for older persons in Europe. Int J Integr Care. 2004, 4: 1-18.
-
Hearn J, Higginson IJ: Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat Med. 1998, 12 (5): 317-332. 10.1191/026921698676226729.
-
Higginson IJ, Finlay IG, Goodwin DM, Hood K, Edwards AG, Cook A, Douglas Hour, Normand CE: Is there show that palliative care teams alter end-of-life experiences of patients and their caregivers?. J Pain Symptom Manage. 2003, 5 (2): 150-168. 10.1016/S0885-3924(02)00599-7.
-
Lorenz K, Lynn J, Morton SC, Dy S, Mularski R, Shugarman Fifty, Lord's day V, Wilkinson A, Maglione Thousand, Shekelle PG: End-Of-Life Care and Outcomes. Evidence Study/Applied science Cess No. 110: AHRQ Publication No. 05-E004-2. 2004, Rockville Doc: Agency for Healthcare Research and Quality
-
Ouwens Grand, Wollersheim H, Hermens R, Hulscher M, Grol R: Integrated intendance programmes for chronically ill patients: A review of systematic reviews. Int J Qual Health Intendance. 2005, 17 (2): 141-146. 10.1093/intqhc/mzi016.
-
MacIntosh J, McCormack D: Partnerships identified within primary health care literature. Int J Nurs Stud. 2001, 38 (5): 547-555. 10.1016/S0020-7489(00)00095-10.
-
Jones 50, Way D: Literature Review Report: Delivering Primary Wellness Care to Canadians: Nurse Practitioners and Physicians in Collaboration. 2004, Ottawa: Canadian Nurses Association
-
Weiss E, Anderson R, Lasker R: Making the nearly of collaboration: Exploring the relationship between partnership synergy and partnership performance. Health Educ Behav. 2002, 29 (6): 683-698. 10.1177/109019802237938.
-
Sullivan TJ: Collaboration: A Wellness Care Imperative. 1998, New York: McGraw-Loma
-
San Martin-Rodriguez L, Beaulieu Doctor, D'Flirtation D, Ferrada-Videla 1000: The determinants of successful collaboration: A review of theoretical and empirical studies. J Interprof Care. 2005, 19 (Suppl ane): 132-147. ten.1080/13561820500082677.
-
Grumbach K, Bodenheimer T: Tin wellness care teams better primary care practice?. JAMA. 2004, 291 (10): 1246-1251. 10.1001/jama.291.10.1246.
-
Zwarenstein Thousand, Goldman J, Reeves S: Interprofessional collaboration: Furnishings of practise-based interventions on professional person do and healthcare outcomes. Cochrane Database of Systematic Reviews. 2009, three.
-
Kelly M, Edwards R, Comello MLG, Plested BA, Jumper-Thurman P, Slater One thousand: The Community Readiness Model: A complementary approach to social marketing. Marketing Theory. 2003, 3 (4): 411-425. x.1177/1470593103042006.
-
Beebe TJJ, Harrison PA, Sharma A, Hedger S: The community readiness survey - development and initial validation. Eval Rev. 2001, 25 (ane): 55-71. 10.1177/0193841X0102500103.
-
Wiener B: A theory of organizational readiness for change. Implement Sci. 2009, iv (67): one-9.
-
Weiner BJ, Amick H, Lee SY: Conceptualization and measurement of organizational readiness for change: A review of the literature in wellness services research and other fields. Med Intendance Res Rev. 2008, 65 (4): 379-436. 10.1177/1077558708317802.
-
Shortell SM, Gillies RR, Anderson DA, Erickson KM, Mitchell JB: Integrating health care delivery. Wellness Forum J. 2000, 43 (half dozen): 35-39.
-
Kelley ML: Developing rural communities' capacity for palliative intendance: A conceptual model. J Palliat Care. 2007, 23 (iii): 143-153.
-
Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century. 2001, Washington DC: National University Printing
-
Bethell C: Patient-Centered Intendance Measures for the National Health Care Quality Report. 2000, Portland: Foundation for Accountability (FACCT)
-
Registered Nurses Association of Ontario (RNAO): Client centred care. 2002, [http://www.rnao.org/Storage/15/932_BPG_CCCare_Rev06.pdf]
-
Audet J, Davis Thou, Schoenbaum SC: Adoption of patient-centered care practices by physicians. Arch Intern Med. 2006, 166 (vii): 754-759. 10.1001/archinte.166.7.754.
-
Cahill J: Patient participation - A review of the literature. J Clin Nurs. 1998, 7: 119-128. x.1111/j.1365-2702.1998.00132.ten.
-
Sainio C, Lauri S, Ericksson Eastward: Cancer patients' views and experiences of participation in care and decision making. Nurs Ethics. 2001, viii: 97-113.
-
Lewin S, Skea Z, Entwistle Five, Zwarenstein M, Dick J: Interventions for providers to promote a patient-centred arroyo in clinical consultations. Cochrane Database of Systematic Reviews. 2001, 4.
-
Edwards RW, Jumper-Thurman P, Plested BA, Oetting ER, Swanson L: Community readiness: Enquiry to do. J Commun Psychol. 2000, 28 (iii): 291-307. 10.1002/(SICI)1520-6629(200005)28:3<291::AID-JCOP5>3.0.CO;2-9.
-
Mattessich P, Monsey B, Murray-Close M: Collaboration: What Makes it Work, second Edition. A Review of Research Literature on Factors Influencing Successful Collaborations. 2001, Saint Paul MN: Fieldstone Brotherhood
-
Accreditation Canada: Hospice palliative care indicators. [http://www.accreditation.ca/accreditation-programs/qmentum/functioning-measures/]
-
Bliss J, Cowley S, While A: Inter-professional working in palliative care in the community: A review of the literature. J Interprof Intendance. 2000, fourteen (3): 281-290. 10.1080/713678572.
-
Palliative Intendance Network Northwest: Hospice palliative care Northwest: The Vision. 2001, [http://bolt.lakeheadu.ca/~necahwww/vision.pdf]
-
Leatt P, Pink K, Guerriere 1000: Towards a Canadian model of integrated healthcare. Healthc Pap. 2000, 1 (2): 13-35.
-
Barrett J, Curran 5, Glynn L, Godwin Yard: CHSRF Synthesis: Interprofessional Collaboration and Quality Master Healthcare. 2007, Ottawa: Canadian Health Services Enquiry Foundation
-
Borrill CS, Carletta J, Carter AJ, Dawson JF, Garrod Due south, Rees A, Richards A, Shapiro D, West MA: The effectiveness of health care teams in the National Health Service. 2001, [http://homepages.inf.ed.ac.uk/jeanc/DOH-last-study.pdf]
-
Barrel G, Markle-Reid Thousand, Browne G: Interprofessional partnerships in chronic illness intendance: A conceptual model for measuring partnership effectiveness. Int J Integr Intendance. 2008, 8: 1-14.
-
Lindeke L, Block D: Interdisciplinary collaboration in the 21st centur. Minn Med. 2001, 84 (6): 42-45.
-
Critchley P, Jadad AR, Taniguchi A, Woods A, Stevens R, Reyno L, Whelan TJ: Are some palliative intendance delivery systems more than effective and efficient than others?. A systematic review of comparative studies. J Palliat Care. 1999, fifteen (4): 40-47.
-
Xyrichis A, Lowton K: What fosters or prevents interprofessional teamworking in main and community intendance? A literature review. Int J Nurs Stud. 2007, 45 (1): 140-153. 10.1016/j.ijnurstu.2007.01.015.
-
Lasker RD, Weiss ES, Miller R: Partnership synergy: A practical framework for studying and strengthening the collaborative advantage. Milbank Q. 2001, 79 (2): 179-205. 10.1111/1468-0009.00203.
-
Arcangelo V, Fitzgerald M, Carroll D, Plumb JD: Collaborative care betwixt nurse practitioners and chief care physicians. Prim Care. 1996, 23 (1): 103-113.
-
Dudgeon D, Knott C, Viola R, Van Dijk J, Preston Southward: Managing Continuity through Collaborative Intendance Plans: A Study of Palliative Care Patients. 2004, Ottawa: Canadian Wellness Services Research Foundation
-
Shaller D: Patient-Centered Intendance: What Does it Take?. 2007, New York: The Republic Fund
-
Ferris FD, Gómez-Batiste X, Fürst CJ, Connor Due south: Implementing quality palliative intendance. J Pain Symptom Manage. 2007, 33 (5): 533-541. x.1016/j.jpainsymman.2007.02.033.
-
Higginson IJ: Wellness Care Needs Cess 2d Series: Palliative and Terminal Care. 1997, Abingdon UK: Radcliffe Medical Press
-
Kristjanson LJ: Validity and reliability testing of the FAMCARE Scale: Measuring family satisfaction with advanced cancer intendance. Soc Sci Med. 1993, 36 (5): 693-701. 10.1016/0277-9536(93)90066-D.
-
Schoot T, Proot I, ter Meulen R, de Witte L: Recognition of client values as a basis for tailored care: The view of Dutch good patients and family unit caregivers. Scand J Caring Sci. 2005, nineteen: 169-176. 10.1111/j.1471-6712.2005.00327.x.
-
Reid R, Haggerty J, McKendry R: Defusing the defoliation: Concepts and measures of continuity of healthcare. 2002, Ottawa: Canadian Wellness Services Research Foundation
-
Nelligan P, Grinspun D, Jonas-Simpson C, McConnell H, Peter East, Pilkington B, Balfour J, Connolly L, Lefebre North, Reid-Haughian C, Sherry K: Client-centred care: Making the ideal real. Hosp Q. 2002, v (4): seventy-74.
-
Bakitas MA, Lyons KD, Dixon J, Ahles TA: Palliative care program effectiveness research: Developing rigor in sampling design, deport, and reporting. J Pain Symptom Manage. 2006, 31 (3): 270-284. 10.1016/j.jpainsymman.2005.07.011.
-
Ellershaw JE, Wilkinson South, (Eds): Care of the Dying: A Pathway to Excellence. 2003, Oxford: Oxford University Printing
-
Ripamonti CI, Farina G, Garassino MC: Predictive models in palliative intendance. Cancer. 2009, 115 (13 Suppl): 3128-34. x.1002/cncr.24351.
-
Bainbridge D, Krueger P, Lohfeld L, Brazil One thousand: Stress processes in caring for an terminate-of-life family unit member: Application of a theoretical model. Aging & Mental Health. 2009, xiii (4): 537-545. ten.1080/13607860802607322.
-
Creswell JW, Plano Clark VL, Gutmann ML, Hanson WE: Advanced mixed methods research designs. Handbook of Mixed Methods in Social and Behavioural Research. Edited by: Tashakkori A, Teddlie C. 2003, Grand Oaks, CA: Sage, 209-240.
-
Johnson RB, Onwuegbuzie AJ: Mixed methods research: A enquiry paradigm whose time has come. Educational Researcher. 2004, 33 (vii): fourteen-26. 10.3102/0013189X033007014.
-
Walshe CE, Cuddle AL, Chew-Graham C, Todd CJ: Instance studies: A research strategy advisable for palliative care?. Palliat Med. 2004, 18 (8): 677-684. 10.1191/0269216304pm962ra.
-
Yin RK: Case Study Research, Design and Methods. 2003, Newbury Park: Sage Publications, 3
-
Ditillo BA: The emergence of palliative care: A new specialized field of medicine requiring an interdisciplinary arroyo. Crit Care Nurs Clin Due north Am. 2002, 14 (ii): 127-132. 10.1016/S0899-5885(01)00002-8.
-
National Informational Committee on Palliative Intendance: Report of the National Advisory Commission on Palliative Care. 2001, Dublin: Republic of ireland Section of Health and Children
-
Wagner E: The office of patient care teams in chronic disease management. BMJ. 2000, 320 (7234): 569-572. 10.1136/bmj.320.7234.569.
-
Dean RA, McClement SE: Palliative intendance research: Methodological and ethical challenges. Int J Palliat Nurs. 2002, 8 (eight): 376-lxxx.
-
McWhinney IR, Bass MJ, Donner A: Evaluation of a palliative care service: Issues and pitfalls. BMJ. 1994, 309: 1340-1342.
-
Kutner JS, Bryant LL, Beaty BL, Fairclough DL: Symptom distress and quality of life cess at the end-of-life: The role of proxy response. J Pain Symptom Manage. 2006, 32 (iv): 300-310. 10.1016/j.jpainsymman.2006.05.009.
-
Durbin J, Rogers J, Macfarlane D, Baranek P, Goering P: Strategies for Mental Health System Integration: A Review - Final report. 2001, Toronto: Ontario Mental Health Foundation
Pre-publication history
-
The pre-publication history for this newspaper tin can exist accessed here:http://www.biomedcentral.com/1472-684X/9/viii/prepub
Acknowledgements
None to exist made.
Author information
Affiliations
Corresponding author
Boosted data
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DB performed the search and analysis of groundwork materials. DB and KB drafted the manuscript. PK, JP, and AT reviewed the manuscript critically for intellectual content. All authors read and approved the final manuscript.
Authors' original submitted files for images
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Admission article distributed under the terms of the Creative Eatables Attribution License (http://creativecommons.org/licenses/by/ii.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and Permissions
About this commodity
Cite this commodity
Bainbridge, D., Brazil, One thousand., Krueger, P. et al. A proposed systems approach to the evaluation of integrated palliative care. BMC Palliat Care nine, 8 (2010). https://doi.org/x.1186/1472-684X-9-8
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/x.1186/1472-684X-9-eight
Keywords
- Palliative Care
- Family Caregiver
- Collaborative Intendance
- Palliative Intendance Service
- Palliative Care Patient
Source: https://bmcpalliatcare.biomedcentral.com/articles/10.1186/1472-684X-9-8
0 Response to "What Is a Systems Approach to Examining a Patient"
Post a Comment